With approval from Health Canada this week and the first shipment of vaccines shipment making landfall in Nova Scotia next Tuesday, the third phase of the coronavirus pandemic is nearly underway.
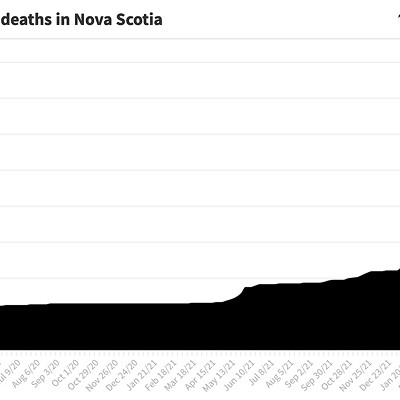
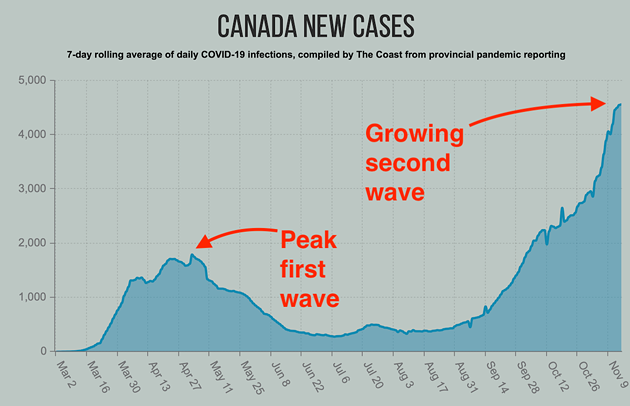
The first phase brought panic and uncertainty: It saw snap-decision lockdowns, confusion over transmission and mounting fear. The second phase saw public health mitigation measures, best-case (Nova Scotia) and worst-case (USA) examples and a global attempt to slow the spread of this virus that no one is immune to—and, to date, has killed 13,000 Canadians.
The introduction of a vaccine (or many vaccines) into public health strategies for fighting Coronavirus Disease changes the game. It means the question is no longer “how long before everyone has been infected and many people have died?” but “how long before everyone has either been infected or vaccinated, and how many fewer people will die?”
Normally, Denys Khaperskyy tells The Coast, it would take four years for a vaccine to make it from its original idea to serving the public. But the scale of the pandemic meant everyone who could rushed to the drawing board and got to work. The Pfizer mRNA vaccine was developed, perfected, put through trials and passed them with no serious side effects. Now—thanks to pandemic protocol from the Canadian government that allowed for results to be reported as they happened—now it’s here.
“This is amazing,” says Khaperskyy, an assistant professor and researcher at Dalhousie University in the department of microbiology and immunology. “It just speaks to the capacity of scientists and humankind in general to adapt and to get things done.”
Amazing indeed. But it’s also normal to look at something that’s never been done before with some reservation. How does it work? How do we know it’s safe? What’s mRNA? Doesn’t the flu shot sometimes kill people? These are all valid questions that we’ve tried to break down for you.
First, for the vaccine itself, Khaperskyy uses the analogy of a book to explain how it works.
In a book, there are letters that make up words that make up phrases that tell you what the book is supposed to be about. With just a single unique phrase, you have no idea what the book is about and couldn’t ever read it start to finish.
In this mRNA text, there are roughly 30,000 letters. It's the same letters (swapping out the U for a T) that are used to describe every gene in our body too, except the text for our genes is much-much longer and is written on 46 long DNA strands called chromosomes.
The scientists who worked on Pfizers’ vaccine figured out a way to make a short mRNA molecule containing just a single word from the text that describes SARS-CoV-2.
This word does not carry enough information to ever become the whole virus, so it could never give you Coronavirus Disease—like how one phrase in a book could never tell you the whole story. But it can be translated by the human body into the building block of a virus (called an antigen) and recognised as something that does not belong.
Because the vaccine containing virus mRNA is injected into the muscle, it is mostly the muscle cells that are doing the translation or copying. Right away, your body—a very sophisticated and smart piece of machinery—recognizes the antigen that is made according to newly introduced instructions as an intruder. It gets to work over the next few days, building and deploying antibodies to neutralize the antigen. This is why you may feel a bit sore and feverish for a day after the injection—because your body is literally fighting off an intruder.
The vaccine works because it causes enough of the SARS-CoV-2 antigen to be made for your body to recognize it as an intruder and practice fighting it off, but it does not contain nearly enough information to generate the whole virus or ever make you sick with COVID.
The injected mRNA is destroyed by the cells in several days and a second shot—a booster—is given to repeat the process and ensure that your body generates an efficient response.
The vaccine does not work instantly, but is ready to go after a few weeks, kicking into action when you’re out in the world and come in contact with the actual SARS-CoV-2 virus.
If your body hasn’t already met the virus—either as an asymptomatic carrier who tested positive or a symptomatic carrier who tested positive and also got sick—then it’s go time. The attack your body sent out against the piece of SARS-CoV-2 you got from the vaccine recognizes its old foe, and is unleashed instantly.
It now has a head start and wins. SARS-CoV-2 has zero time to get anywhere near making you sick, you don’t get Coronavirus Disease, and you’re now immune to COVID-19. We still don’t know how long the immunity lasts (months or years), or if this means you can’t pass the virus on without getting sick, so that’s why social distancing and masks will still be needed until everyone’s been vaccinated. (For this info in video form, watch this.)
Understanding how it works in your body is one thing, but understanding how governments weigh the risks and benefits of these kinds of things when it comes to public health is another.
In the detailed document Health Canada rolled out on Wednesday outlining its plan for the vaccines, it included the note that “Adverse events are to be expected, and will not necessarily change the risk/benefit profile of the vaccine.”
But why would adverse reactions—a risk to the individual person taking the vaccine—not change the government’s decision to continue using it?
“The short answer to that,” explains Khaperskyy, “is because the body is complicated. And because even though we are all similar, we are all humans, no body is like any other body. Everyone's unique.”
The longer answer lives on a spectrum of risk versus reward. The mission of a vaccine is to ensure a desired effect is achieved safely. The desired effect, in this case, is resistance to a virus that a year ago no one had ever heard of. Achieving it safely balances the risk of the virus and the disease it causes with the potential risks a vaccine entails.
“If there is no effect, then having a safe vaccine that does not protect would not be acceptable,” says Khaperskyy. “That's the bad extreme on one side. On the other side the extreme is that the vaccine protects everyone [from COVID-19], but a lot of people would have adverse reactions, so it would be unacceptable because your risks of becoming sick from getting the vaccine is just too high.”
The new technology, Khaperskyy says, is a far cry from the first vaccines—and much safer. In the smallpox days, he says, people would take the scabs of someone who had smallpox and inject that into a healthy person, essentially giving them smallpox—the equivalent of giving them the entire book, not just one phrase. The idea was that the scab was a small enough dose that the body would learn how to fight it, so when it came in contact with smallpox out in the world it would remember how to fight and win. These inoculations could have given smallpox to one out of 10 people while protecting only 9, but the admittedly imperfect practice stuck because chances of dying from smallpox were much higher. In the game of public health, it really is about math.
“We are miles, light years away from that, in terms of what we know, what comes as a component of quality control and what's expected to happen,” says Khaperskyy about how far away the science behind the smallpox vaccine is. But it still comes down to math. In some ways it’s grim, but to deny it’s what’s happening is also not helpful. And every decision made by government in Canada for fighting the pandemic can be brought back to some weighing of the pros and cons.
In this case, Khaperskyy says the risks of getting vaccinated—like soreness, an allergic reaction or the rare possibility of a severe reaction—are simply incomparable when compared to risk of getting COVID-19. (Not to say there isn’t always a human being on the other end of the phrase minimal risk).
The Pfizer vaccine was tested on 42,000 people. Six percent of those people had allergic reactions to the vaccine. Zero percent had a seriously bad reaction to the vaccine—that’s what allowed it to be approved by Health Canada following all the normal protocols for vaccine approval.
An allergic reaction isn’t good, but unintentionally spreading COVID-19 to someone who ends up dying from it is worse. So in this case, the risk of getting an allergic reaction is overridden by the vaccine’s probability to prevent you from dying of Coronavirus Disease. In the case of pregnant people, none of the 42,000 people in the original study were pregnant, so we don’t know if any adverse effects could occur. Is there any way to know about the adverse effects of the vaccine on pregnancies without pregnant people taking the vaccine? Not really. Can we mitigate that by ensuring pregnant people avoid situations that could allow for spread of the disease? Yep. It’s still all just checks and balances. Human survival math.
If—in a hypothetical situation made up by this reporter for the sake of understanding risk versus reward using fake numbers—if the Pfizer vaccine trial ended up causing one person’s death, it would still kill fewer human beings if injected into every person on earth than COVID-19 will if it continues at its current pace. Lucky for us, if it had killed someone in its trial, we would not be seeing it rolled out in provinces across Canada next week.
The people who have the greatest risk of catching the virus and dying from COVID-19 are at the top of the list to receive a vaccine. This is another layer of the risk versus reward equation. In Nova Scotia, starting next Tuesday, that’ll be 1,950 Nova Scotians who are working in COVID-19 care units, Regional Care Units and intensive care units that care for COVID-19 patients. In the first three months of 2020, the province is expecting to receive 150,000 doses, enough for 75,000 people to receive the required two doses each.
As more vaccines become available—the Moderna vaccine, which uses the same technology as the Pfizer vaccine and is still working through the end phase of its trials—doses will be doled out in order of priority. That priority matrix is also a balancing act. Young healthy people have a lower risk of dying from COVID-19, but for those who work with COVID-19 patients, being young and healthy isn’t enough to guarantee safety, so they move up the priority ladder.
Nova Scotia said in a release this week it’d start, like the rest of Canada, with long-term care residents and staff, seniors who live in the community beginning with those who are over 80 years of age, then people over 75 and then people over 70 and health-care workers directly involved in patient care.
“The vaccine is going to make a huge difference,” said Nova Scotia's chief medical officer Robert Strang on Friday, “we know that. But the uncertainty around when you’re going to get it and when you’ll be eligible, I get that that causes anxiety.”
Strang assured Nova Scotians that the rollout would be logical and evidence-based, adding that it will take a number of months before everyone has the chance to be vaccinated. The news of vaccines brings us to the third phase of the pandemic, where the goal is to see the number of cases—and deaths—go down, as the number of people vaccinated goes up, until pretty much everyone has been vaccinated or has gotten the virus and didn’t die.
“So,” he says “the faster everyone gets vaccinated, the better.”
As more people around the globe take the vaccine, what we know about it will increase. As Khaperskyy said, bodies are unique. And 42,000 people is a lot of people, but the world has 7.8 billion people on it—every single one of whom has no built-in defence to SARS-CoV-2 and Coronavirus Disease. Like our understanding of how to slow the spread of Covid got better with time, our understanding of how to best vaccinate people will get better, too. People who want to wait and see if the vaccine affects fertility or a specific unique health condition their unique body has will have some time to do so—early projections for vaccine availability in Canada mean we won’t see everyone vaccinated until the end of 2021.
But Khaperskyy says that is still something worth celebrating.
Imagine if "no one cared about the vaccine,” he says, “there would be no end in sight for this pandemic. People would keep dying and there would be no hope. But now we have a hope.”