Nova Scotia’s health minister stopped short of describing the province’s latest health spending announcement as a “blank cheque,” but that might as well have been the message Wednesday as premier Tim Houston’s government shared its latest plans to “go like hell” in addressing a health-care system sorely in need of mending.
On Jan. 18, health minister Michelle Thompson and Nova Scotia Health CEO Karen Oldfield unveiled a laundry list of changes to how the province aims to improve the functioning of emergency health care across the province. On the fix-it list? Quicker ambulance response times, specialized doctor-led teams to triage patients arriving at ERs, virtual care for patients clogging ERs with non-emergencies and real-time data on where to find hospital beds. All for somewhere in the neighbourhood of “tens of millions” of dollars, Nova Scotia’s deputy minister of health, Jeannine Lagassé, told reporters.
The announcement comes as welcome news for Nova Scotia’s overburdened health-care system, but questions remain: How quickly can the province implement its envisioned changes? What solutions has Houston’s government overlooked? And do Wednesday’s announcements address the health-care system’s root issues, or merely its most visible symptoms?
Timeline for action
Both Oldfield and health minister Thompson stressed the urgency of tackling the province’s health-care crisis in Wednesday’s announcement.
“We cannot take our foot off the gas,” Thompson told reporters. Oldfield described the pressure from the premier’s office as a “firehose,” with a memo to “move, move, move” on implementing change.
What that means in the near term, at least in part, is additional nurse practitioners and physician assistants staffing emergency departments. The province says those roles will begin immediately at both the Dartmouth General Hospital and South Shore Regional Hospital. But it’s not clear how the province will recruit for those roles—or how many nurse practitioners and physician assistants Nova Scotia Health could actually deploy today, if it wanted to.
The province says patient advocates—which offer ER patients company and conversation while they’re waiting to be seen—will be in every emergency department by Saturday. Some had already been in place before the COVID-19 pandemic, the CBC reports. But most of those roles, which had previously been volunteer-based, will now be paid.
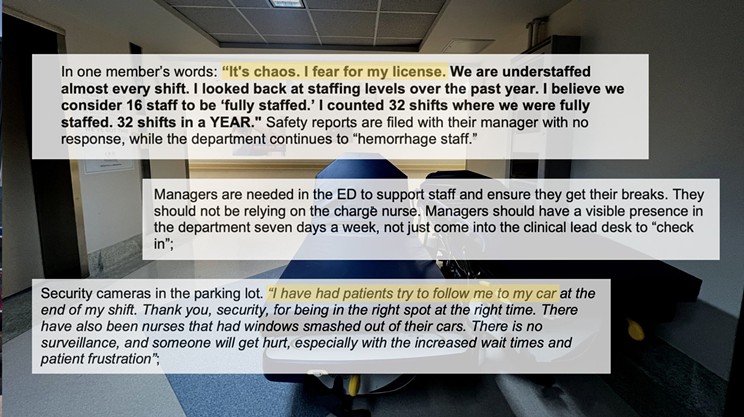
Nurses’ union leader ‘not seeing much for nurses’ in latest announcement
Janet Hazelton has followed the province’s health-care promises with interest. As president of the Nova Scotia Nurses’ Union (NSNU) since 2002, Hazelton has watched her colleagues shoulder 12-hour shifts “that turn into 16 and 18 and 24 [hours]” because there aren’t enough nurses to go around on a ward.
Reading through Wednesday’s provincial announcement, Hazelton tells The Coast she’s “not seeing much” that will improve her nursing peers’ working conditions.
“You can recruit [new positions] until forever, but if you don’t figure out a way to retain, it doesn’t matter what your recruitment efforts look like,” she says. “It’s keeping them once they’re there.”
She’d like to see tuition relief offered to students who pursue nursing—“if I’m looking at a bill of probably $125,000, that's a lot of money,” Hazelton says—provided that those nurses agree to work in the province once they’ve completed their training.
There’s already precedent to follow. The province’s latest announcement offers a $11,500 tuition rebate for paramedics who agree to work in the province for at least three years.
Health system ‘neglected for years,’ minister says
Both Thompson and Oldfield were keen Wednesday to position the health-care crisis as one their administration had inherited, not worsened. Nova Scotia’s health-care system “was built during a different era,” Oldfield said in a release, “and aside from technological advances, it has barely changed since.” Thompson told reporters that the province’s health-care system had been “neglected” for “almost my entire career as a registered nurse,” and that despite calls from health-care workers “that the system was in trouble… nobody listened.”
“No one person can move this mountain by themselves,” Oldfield added. “We can do it if we all pull together with a common goal: a system that is ready, responsive and reliable.”
On some level, Hazelton agrees.
“I think everyone wants the best for Nova Scotians,” she tells The Coast. “Everybody realizes that we have a huge issue to fix… It's just how do we get there?”
Per Nova Scotia Health’s latest public reporting, 97.6% of the province’s acute and non-acute hospital beds are full. And some hospital units across Nova Scotia have up to 80% nurse vacancy rates.
Shift to prevention over crisis response?
N Leger Siritsky has seen Nova Scotia’s ER crisis play out before. Now an advocacy consultant with the Nova Scotia College of Social Workers, Siritsky formerly served as the vice-president of KentuckyOne Health, a public hospital system in Louisville. There, the issues were much the same: Emergency waits were a problem. Patients were leaving the hospital in search of other options. And the system’s pressures meant that both patients and staff were left feeling unsafe.

Siritsky worked to redesign the hospital’s emergency departments “to make sure that everyone’s voice and perspective is included.” One of the primary takeaways was to shift from crisis response to prevention—and from a medical model that prioritizes doctors to one using team-based care.
“Doctors and nurses are burning out,” Siritsky tells The Coast. “Meanwhile, there's really effective ways to integrate chaplains, social workers, occupational therapists and peer support specialists into the mix so that doctors can work at their highest level.”
That applies to the emergency department, but beyond it, too. Both Siritsky and Hazelton point to a significant share of patients (“sometimes it’s 50 to 60%,” says Hazelton) who are arriving at ERs because they can’t access primary care. Finding ways of meeting those health needs outside of a hospital setting could free up room for ER patients with more urgent needs to be seen faster—and to not fall through the cracks.